Terminal sterilization is the process of sterilizing aseptic products, such as medical devices, pharmaceuticals, and food products after they have been packaged in a sterile environment. This method of sterilization involves exposing the products to high heat, radiation, or chemicals to kill any remaining microorganisms that may be present. Terminal sterilization is a critical step in ensuring the safety and efficacy of these products, as it eliminates the risk of contamination and helps to extend their shelf life.
GMP guidelines Guidance about the Terminally Sterilized Products
Annex 4 of the Good Manufacturing Practice (GMP) guidelines provides detailed guidance on the terminal sterilization of aseptic products. According to this annex, terminal sterilization is a critical step in ensuring the safety and efficacy of aseptic products and must be carried out in compliance with the relevant GMP regulations.
The annex outlines several methods for terminal sterilization, including moist heat sterilization, dry heat sterilization, radiation sterilization, and sterilization by gas. Each method has its own specific requirements and limitations, and the appropriate method must be selected based on the nature of the product and its intended use.
The GMP guidelines also specify the validation requirements for terminal sterilization processes, including the need for comprehensive validation studies to establish the effectiveness and reproducibility of the process. In addition, the guidelines require that the sterilization process be monitored and controlled to ensure consistent and reliable sterilization of each batch of product.
Overall, compliance with Annex 4 of the GMP guidelines is critical for ensuring the safety, efficacy, and quality of terminal sterilized aseptic products. By following these guidelines, manufacturers can help to minimize the risk of contamination and ensure that their products meet the highest standards of quality and safety.
Why pharmaceuticals products need terminal sterilization.
Pharmaceutical products need terminal sterilization of a sterile product to eliminate any remaining microorganisms that may be present in the product and to ensure its safety, efficacy, and stability.
During the manufacturing process, pharmaceutical products are typically prepared in a sterile environment to prevent contamination by microorganisms. However, even with the use of aseptic techniques, there is always a risk of contamination. Therefore, terminal sterilization is a critical step to ensure that any microorganisms that may have survived the aseptic processing are killed.
If a pharmaceutical product is contaminated with microorganisms, it can lead to serious health risks for the patients who use it. For example, contaminated injectable products can cause serious infections, while contaminated ophthalmic products can cause eye infections. Therefore, it is essential to ensure that pharmaceutical products are free from microorganisms before they are released for use.
Terminal sterilization also helps to extend the shelf life of pharmaceutical products by preventing the growth of any microorganisms that may have survived the manufacturing process. This helps to ensure that the product remains safe and effective for use over a longer period of time.
In summary, terminal sterilization is an important step in ensuring the safety, efficacy, and stability of pharmaceutical products. By eliminating any remaining microorganisms, it helps to reduce the risk of contamination and ensures that the product meets the highest standards of quality and safety.
Terminal sterilization definition
Terminal sterilization refers to the process of sterilizing a product, typically in its final container, to eliminate any microorganisms that may be present and ensure its safety, efficacy, and stability. The goal of terminal sterilization is to achieve a product that is free from viable microorganisms, including bacteria, viruses, and fungi. This process is typically performed using methods such as heat, radiation, or chemical sterilization, and is critical for ensuring that products such as medical devices, pharmaceuticals, and food products are safe and effective for use.

What is terminal sterilization?
Terminal sterilization refers to the process of sterilizing a product, typically in its final packaging, to eliminate all microorganisms, including bacteria, viruses, and fungi, and ensure the product’s safety and efficacy. The goal of terminal sterilization is to achieve a product that is free from viable microorganisms, which may cause infections or other adverse effects when used.
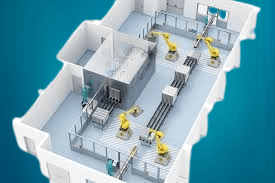
Terminal sterilization is an essential step in the manufacturing process of many products, including medical devices, pharmaceuticals, and food products. The process may be carried out using various methods, such as moist heat sterilization, dry heat sterilization, radiation sterilization, and sterilization by gas. The method used depends on the nature of the product and its intended use.
In addition to eliminating microorganisms, terminal sterilization helps to extend the shelf life of products by preventing the growth of any remaining microorganisms that may have survived the manufacturing process. By ensuring the safety and stability of products, terminal sterilization helps to protect the health and well-being of consumers.
Terminal sterilization vs aseptic processing
| Details | Terminal Sterilization | Aseptic Processing |
| Definition | Preparing products in a sterile environment to prevent contamination by microorganisms | Preparing product in a sterile environment to prevent contamination by microorganisms |
| Method | Heat, radiation, chemical sterilization | Cleanrooms, isolators, specialized equipment, and techniques |
| Materials | Careful selection of packaging and sterilization materials required | Careful selection of materials required |
| Applicable Products | Products that can withstand high temperatures or chemical exposure | Products that cannot withstand high temperatures or chemical exposure |
| Advantages | Highly effective in achieving sterility, suitable for a wide range of products | Protects the product from damage during sterilization, suitable for sensitive products |
| Disadvantages | Requires careful selection of materials and packaging, may compromise product quality | Requires specialized equipment and techniques, can be expensive |
| Examples | Pre-filled syringes, surgical instruments | Biologic drugs, vaccines, creams, and lotions |
Terminal sterilization methods include
There are several terminal sterilization methods that can be used to achieve sterilization of a product, including:
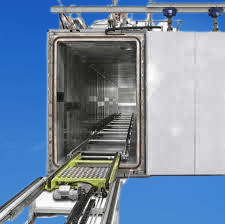
- Steam sterilization: This method uses high-pressure steam to sterilize products and is one of the most commonly used methods in pharmaceutical manufacturing.
- Dry heat sterilization: This method uses dry heat to sterilize products and is typically used for products that cannot withstand high-pressure steam.
- Radiation sterilization: This method uses ionizing radiation (e.g., gamma radiation) to sterilize products and is typically used for products that cannot withstand heat.
- Chemical sterilization: This method uses chemical agents such as ethylene oxide or hydrogen peroxide to sterilize products and is typically used for heat-sensitive products.
The choice of method(s) depends on various factors, including the nature of the product, its intended use, and the available resources and expertise. Each method has its own advantages and limitations and must be carefully selected and validated to ensure that it is effective in achieving sterilization while maintaining the quality of the product.
Critical Parameters of Terminal Sterilization
Critical parameters of terminal sterilization typically include temperature, exposure time, pressure (for steam sterilization), dosage (for radiation sterilization), and the F0/FH value. Let’s delve into these parameters, their calculations, and the FZ value:
- Temperature: Temperature is a crucial parameter in terminal sterilization processes. It determines the rate of microbial destruction. For steam sterilization, typical temperatures range from 121°C to 134°C.
- Exposure Time: The exposure time is the duration for which the product is subjected to the sterilization process. It depends on the nature of the product and the chosen sterilization method. Longer exposure times generally increase the efficacy of sterilization.
- Pressure (for steam sterilization): In steam sterilization, pressure is maintained to achieve the desired temperature. The pressure is typically controlled within a range specified for the sterilization process (e.g., 1.5 – 2 bar).
- Dosage (for radiation sterilization): Dosage refers to the amount of ionizing radiation (e.g., gamma rays) required for sterilization. It is measured in Grays (Gy) or kiloGrays (kGy). The dosage depends on the radiation sensitivity of the product and is determined through validation studies.
- F0/FH Value: The F0 value (pronounced as “F-zero”) is a measure of the lethality of a sterilization process using heat. It represents the time equivalent at a reference temperature that achieves the same microbial destruction as the actual process. The F0 value is calculated using a mathematical formula based on temperature and time. Similarly, the FH value is used in moist heat sterilization (e.g., steam sterilization) and considers the effects of both temperature and humidity.
Calculation of F0/FH Value: The F0 value can be calculated using the following formula:
F0 = (t – tref) * 10^(T-121.1)/z
where: F0 = F0 value (in minutes)
t = Total exposure time (in minutes)
tref = Reference exposure time (in minutes) at the reference temperature
T = Temperature during sterilization (in °C)
z = Decimal reduction time (D-value) of the target microorganisms at the reference temperature
The FZ value is the lethality equivalent to the F0 value, but it is used for moist heat sterilization. The FZ value incorporates the effects of temperature and humidity during the sterilization process.
It is important to note that the specific calculations and parameters may vary depending on the sterilization method and industry standards. Validation studies and regulatory guidelines should be followed to determine the appropriate critical parameters for each specific sterilization process.
Terminal sterilization guidelines
Terminal sterilization guidelines provide recommendations and requirements for the proper sterilization of products, ensuring their safety, efficacy, and compliance with regulatory standards. While specific guidelines may vary depending on the industry and regulatory body, here are some general principles and considerations commonly found in terminal sterilization guidelines:
- Validation: Terminal sterilization processes must undergo thorough validation studies to demonstrate their effectiveness in achieving sterility. This includes establishing appropriate sterilization parameters, verifying equipment performance, and conducting microbial challenge testing.
- Packaging: Proper packaging is crucial to maintain sterility throughout the sterilization process and subsequent storage. Guidelines often specify requirements for packaging materials, integrity testing methods, and appropriate sealing techniques to prevent recontamination.
- Sterilization Method Selection: Guidelines may outline suitable methods for different product types, considering factors such as product composition, sensitivity to heat or radiation, and container materials. Common methods include steam sterilization, dry heat sterilization, radiation sterilization, and chemical sterilization.
- Sterilization Parameters: Guidelines provide recommendations for the appropriate sterilization parameters, such as temperature, exposure time, pressure, and dosage, depending on the selected sterilization method. These parameters must be established based on scientific evidence and validated through experiments.
- Bioburden Control: Effective bioburden control measures, including cleaning, disinfection, and environmental monitoring, are essential prior to sterilization to minimize microbial load and enhance sterilization efficacy.
- Sterility Assurance Level (SAL): Guidelines often define the required level of sterility assurance, typically expressed as the probability of a non-sterile unit within a given population (e.g., SAL of 10^-6, which means one non-sterile unit per one million units).
- Process Monitoring: Guidelines recommend implementing robust process monitoring and control measures during terminal sterilization. This may include routine temperature and pressure monitoring, biological indicator testing, and documentation of process parameters.
- Quality Control and Documentation: Adequate documentation and record-keeping are essential to demonstrate compliance with sterilization guidelines. This includes batch records, sterilization logs, validation reports, and quality control testing results.
It is important to consult specific regulatory guidelines applicable to your industry, such as those issued by the FDA, EMA, or ISO, for detailed and up-to-date recommendations on terminal sterilization practices.
Terminal sterilization vs disinfection
| Factor | Terminal Sterilization | Disinfection |
|---|---|---|
| Objective | Complete elimination of all viable microorganisms. | Reduction of microbial load to a level considered safe. |
| Microbial Kill | Eliminates all viable microorganisms, including spores. | Reduces the number of microorganisms, but may not eliminate all. |
| Method Effectiveness | Highly effective in achieving sterility. | Effective against a broad range of microorganisms, but may not eliminate all. |
| Application | Applied to sterile products or surfaces intended for injection, infusion, or implantation. | Applied to non-sterile surfaces, equipment, or objects. |
| Level of Assurance | High level of sterility assurance (e.g., SAL of 10^-6). | Provides a certain degree of microbial control and risk reduction. |
| Process Validation | Requires rigorous validation studies to demonstrate the effectiveness. | Validation may be less complex and may not require sterility testing. |
| Examples | Steam sterilization, dry heat sterilization, radiation sterilization. | Chemical disinfectants (e.g., alcohol, quaternary ammonium compounds), UV light disinfection, bleach solution. |
Frequently Asked Questions:
What is the purpose of terminal sterilization in the manufacturing of sterile products?
Answer: The purpose of terminal sterilization is to eliminate all viable microorganisms from a product, ensuring its safety and efficacy.
What are the commonly used methods for terminal sterilization?
Answer: Common methods include steam sterilization, dry heat sterilization, radiation sterilization, chemical sterilization, and filtration sterilization.
How does steam sterilization work?
Answer: Steam sterilization, also known as autoclaving, utilizes high-pressure saturated steam to achieve sterilization by denaturing proteins and destroying microorganisms.
What are the advantages of radiation sterilization?
Answer: Radiation sterilization can effectively sterilize heat-sensitive products without causing significant temperature rise or altering product characteristics.
How is the sterilization cycle for terminal sterilization determined?
Answer: The sterilization cycle is determined through validation studies, considering factors such as product characteristics, container materials, and regulatory requirements.
What is the difference between aseptic processing and terminal sterilization?
Answer: Aseptic processing involves preparing a product in a sterile environment to prevent contamination, while terminal sterilization is the process of sterilizing a finished product.
How is the effectiveness of terminal sterilization validated?
Answer: The effectiveness of terminal sterilization is validated through rigorous testing, including microbial challenge studies, sterility testing, and process validation studies.
What is a biological indicator in terminal sterilization?
Answer: Biological indicators are test systems containing a known number of microorganisms used to validate the sterilization process. They serve as a direct indicator of microbial destruction.
How is the sterility of a product determined after terminal sterilization?
Answer: Sterility testing is performed using appropriate methods, such as membrane filtration or direct inoculation, to confirm that the product is free from viable microorganisms.
What are some critical considerations for selecting the appropriate terminal sterilization method?
Answer: Factors to consider include product characteristics, compatibility with packaging materials, regulatory requirements, product stability, and potential impact on product quality.

Can I use the same autoclave to sterilize components(SS tool, tweezers and empty containers) and final product in vials or ampoules?
Yes, all the components are the same, only inside trays are designed to kept ampoules or vials. You may sterilize all components too.
You May also read about the autoclave to sterilize components(SS tool, tweezers and empty containers) https://flairpharma.com/working-principle-of-autoclave/